When I first started this journey, I knew practically nothing about data in the mental health and addictions sector. So when I was asked to co-lead a Data and Performance Measurement Strategy with Dr. Paul Kurdyak, I was concerned about my limited knowledge of this subject.
But it turned out that no one else knew anything either – data in the mental health and addictions sector was a complete mystery. So we began our journey with a simple question: What does the data landscape for the mental health and addictions sector look like in Ontario?
As a first step, we laid out the general continuum of care for mental health and addictions services in Ontario.
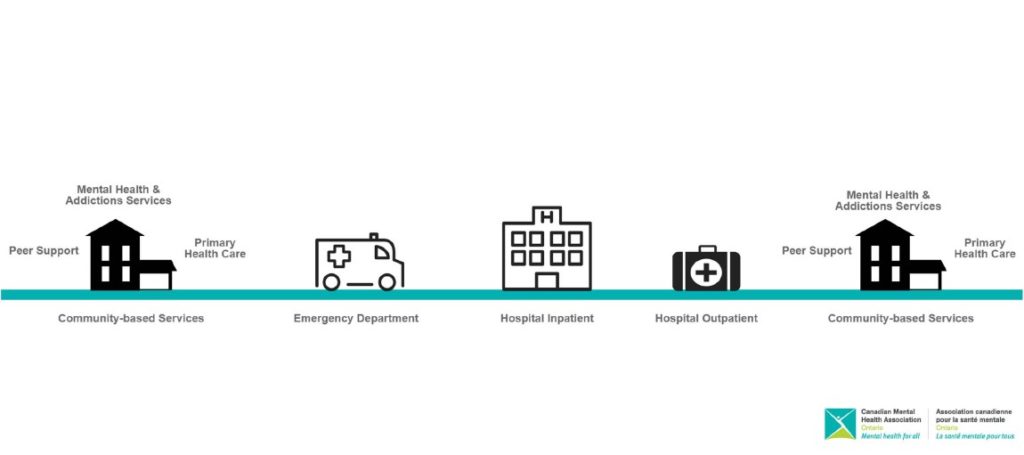
In most cases, people with lived experience (PWLE) of mental health and addictions issues access services in the community. This could be through their family doctor or other primary health care provider like a community health centre, through a community-based mental health and addictions organization such as Canadian Mental Health Association, as well as through peer-led organizations such as Sound Times.
When an individual experiences a mental health or addictions related crisis, they might access services through a hospital emergency department such as the Centre for Addiction and Mental Health. This may lead to accessing services as an in-patient, then as an out-patient, and then back out into the community for follow-up care.
Based on this general continuum of care, we then identified all of the different provincial-level data repositories that capture mental health and addictions related patient information.
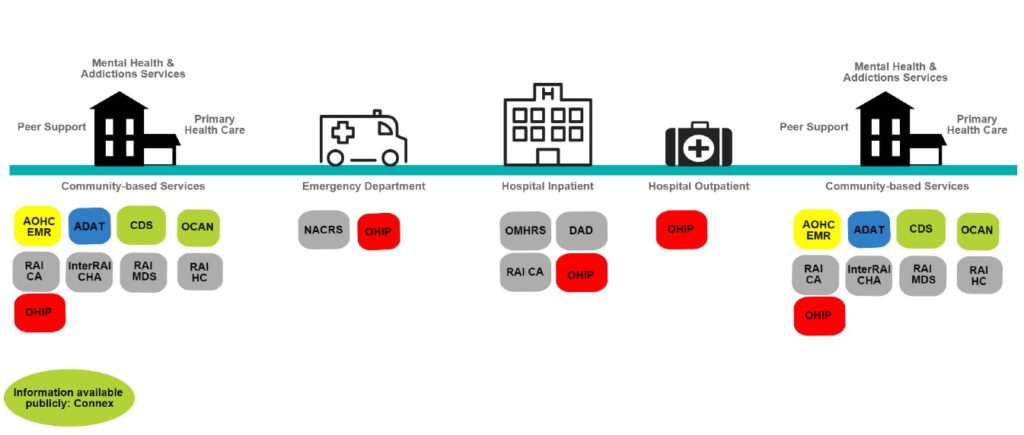
During this process, we uncovered that there are relatively few data repositories in the hospital sector, compared to the cluster in the community mental health and addictions sector (many of these data repositories are examined in other articles). This is when the complexity of the data landscape first began to surface.
A “Giant Mess”
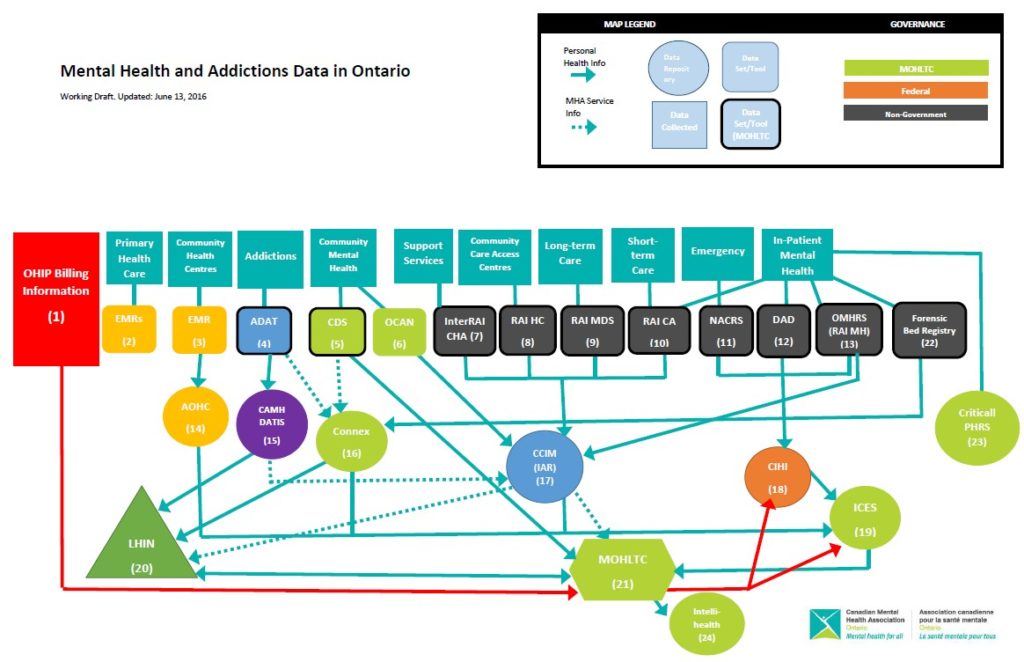
Our next step was to identify who has access to these data repositories and determine the flow of information. What we discovered was a giant mess, with many winding roads and dead ends. We developed a data roadmap to help us visualize the information pathways only to realize that not all roads led to the Ministry of Health and Long-Term Care or to the Local Health Integration Networks (LHINs). In fact, not one single organization or individual in Ontario had the ability to see all of the data across the continuum of care for mental health and addictions services.
Not being able to see all of the data restricts the ability to make informed, evidence-based decisions. From a health systems policy perspective, this means government is unable to measure the impact of financial investments made in mental health and addictions nor focus future investments on services and supports that are achieving good patient outcomes. Furthermore, without access to all data, it’s impossible to compare performance across organizations (in both community and hospital) and see outcomes across the system.
When one single entity is not able to see all of the information, that means there is no single entity making the decisions. This results in the system moving in multiple directions without a clear pathway forward. This is incredibly problematic. This is what fuels the fractured system of mental health and addictions care in Ontario.
Gaining Clarity in a Cloudy Data Landscape
So how do we chart a course forward? This was the enormous task-at-hand for the Mental Health and Addictions Leadership Advisory Council, the advisory body to government on the implementation of Ontario’s Comprehensive Mental Health and Addictions Strategy.
In July 2015, the council convened a Data and Performance Measurement Reference Group comprising experts in health systems data and performance measurement, health and public policy, mental health and addictions community agencies and hospitals, and PWLE. From that body, a small task group was struck to carry the work forward.
The task group held extensive consultations across the mental health and addictions sector, with service providers and service users, to inform our work. A total of 350 people were consulted, including 10 in-person meetings, three webinars, and an online survey, and an additional 400 people were engaged through conference presentations. These consultations were extremely valuable as it revealed many data challenges across the system.
At an agency level, stakeholders identified that there is an immense documentation burden and time commitment required to complete data collection and reporting requirements which leads to time away from clinical care. There is also a lack of data infrastructure and lack of capacity in the collection, analysis and utilization of data across many agencies in the community sector as well as some small, rural and northern hospitals.
At a LHIN level, there is a lack of consistency and standardization of data across all LHINs, which leads to challenges in obtaining comparable information across regions. At a provincial level, there is a lack of evidence-based performance indicators for the mental health and addictions sector across the continuum of care.
A Path Forward Emerges
After hearing about the challenges in the system, the task group began to chart a course forward. We rolled up our sleeves and began navigating the road ahead with an end goal to build a comprehensive data and performance measurement strategy for the mental health and addictions system in Ontario.
Vision for Ontario:
A high-performing mental health and addictions system that is appropriately resourced and accountable to the public ensures that services and supports are provided in a safe, effective, client-centred, timely, efficient and equitable manner.
It began with development of a vision for the mental health and addictions sector. And the task group agreed that the vision was to be centred on the principles of health quality improvement.
The task group then developed a scorecard of standard performance indicators for the mental health and addictions system, across the continuum of care.
These indicators are measurable and yield results that are interpretable (gives meaningful insights into the overall functioning of the system) and actionable (gives agencies the ability to take action to improve quality of care).
And, finally, the task group produced a step-by-step plan for data, performance measurement and improvement.
However, there is one vital and critical step that is most important. And that is to centralize data governance and oversight for the mental health and addictions system. The task group recommends establishing a single entity to centralize data governance oversight that can:
- coordinate and integrate the existing mental health and addictions data and information systems;
- develop and implement data standards;
- address key gaps in existing data collection platforms; and,
- oversee and facilitate the use of data in performance measurement and improvement.
This recommendation was validated and endorsed by the Mental Health and Addictions Leadership Advisory Council and became a keystone of its 2016 annual report. Strong centralized leadership driven from meaningful cross-sectoral collaboration and engagement is needed to drive results and navigate through the existing fractured system.
The journey to this comprehensive data and performance measurement strategy took 12 months, included immense cross-sectoral collaboration across the continuum of care, and some blood, sweat and tears, too. As I look back, I realize that we are just at the beginning of the journey to achieving a high performing system – but at least this time we will start the journey with a roadmap in hand and a clear course forward.
Uppala Chandrasekera is the Director, Public Policy at CMHA Ontario and the Co-Chair of the Data and Performance Measurement Task Group of Ontario’s Mental Health & Addictions Leadership Advisory Council.
