To provide high quality mental health and addictions care for clients, and to plan for a system that facilitates this care, meaningful information is required. More specifically, better understanding of clients, their individual needs, and the outcomes of their care are pivotal to providing high quality mental health and addictions services.
However, simply improving the data reporting among mental health and addictions agencies is not the answer. More data collection alone will not provide enough information to design the best care for our clients.
High quality care requires us to consider the full needs of our patients. And measuring mental health care across the entire healthcare system is essential to doing just that.
Step One – Good Quality Data in Community Mental Health and Addictions Agencies
High quality care starts with having an improved understanding of the services clients are receiving – within and across mental health and addictions agencies. This requires standardizing what the community measures and being able to compare and consider service activity across mental health and addictions organizations.
Community Business Intelligence (CBI) is an example of a system that does just that. The CBI system allows the Toronto Central Local Health Integration Network (LHIN) and its health service providers – mental health agencies, addictions agencies and community support service agencies – to track individual clients across the community sector.
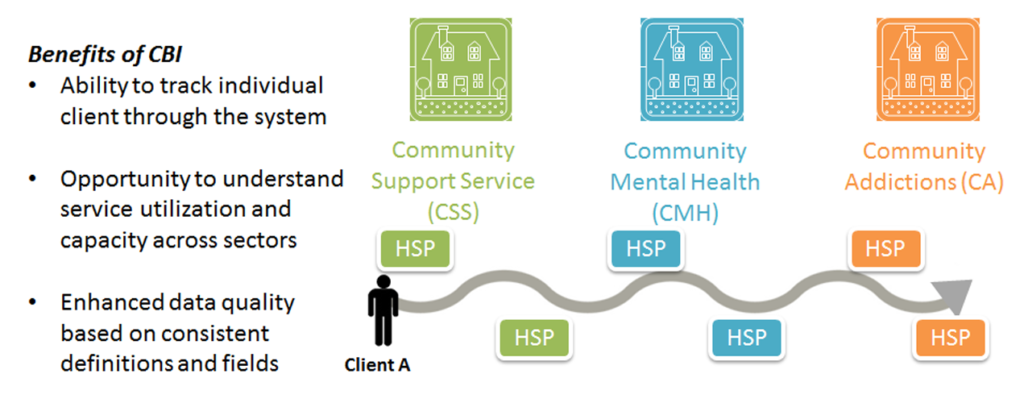
Mohamed Badsha, Chief Executive Officer of Reconnect Community Health Services, notes that CBI was built to address gaps in existing information for community mental health, community addictions and community support services client information.
“Currently in Ontario, only the Toronto Central LHIN can answer these questions: what is the real-time capacity and utilization for all community-funded services, what are client wait times for community programs, where are people living who are accessing services, who is using services, when and which services and for how long and what combination of services are they using?”
Step Two – Connect Data to Get a Complete Picture
Patients with mental health and addictions conditions have different interactions with the health care system. They receive care for their mental health or addictions issue and for other physical health conditions. When we measure mental health and addictions services in a standardized way that is interpretable across other aspects of the broader health care system, we can link the data and understand the full client journey. This might mean understanding the intersection of the patient experience as they receive service with their primary care doctor, in hospital, or in the community.
The Institute for Clinical Evaluative Sciences (ICES) conducts these analyses. And for patients who receive community mental health and addictions care in the Toronto Central LHIN, ICES and CBI analyze how the patient’s mental health and addictions care is linked to both acute care (i.e. hospital) and primary care (i.e. family doctor). Through these efforts, we can start to answer questions about who is being discharged from hospital, what kind of community care are they receiving, and what is the impact of the services they receive?
This type of work is increasingly important with the emergence of the Patients First Act in Ontario. Under the act, LHINs will be further aligning and integrating programs and services for local populations, and they’ll require robust information about the intersecting health needs of their communities.
High quality mental health and addictions data is part of the critical foundation of sound planning and decision-making.
Sophia Ikura, Toronto Central LHIN’s Senior Director of Strategy, Community Engagement and Population Health explains that “planning for population health requires an understanding of community needs and how services can be designed to improve access and quality of care.”
“High quality mental health and addictions data is part of the critical foundation of sound planning and decision-making,” Ikura says.
Step Three – Remember, Care Happens in all Kinds of Settings
People with mental health and addictions conditions seek treatment in a variety of settings: community agencies, primary care, hospitals and long-term care. As a healthcare system, we want to ensure that no matter where someone receives care, the service received is evidence-based. To do this, we need to measure the same outcomes in multiple settings.
Over the past 18 months, a collaboration between community hospitals, family health teams and academic hospitals is demonstrating the success of just such an approach with the implementation of the DA VINCI (Depression and Alcohol – Validation of an Integrated Care Initiative) project.
With support of a grant through Health Quality Ontario and the Council of Academic Hospitals of Ontario, the DA VINCI project has led to the implementation of an integrated care pathway for major depression and alcohol use disorder across nine sites in the province. In every case, the same clinical assessment tools are used and the same outcomes measured. And across the board, positive outcomes were observed.
The takeaway: the more we measure the same things across health care settings, the more we learn about the kind of patients we are treating and which treatments are most effective.
Step Four – Evolve What We Measure
As a sector, we know we need better data to plan and provide the best quality care for the people we serve. However, this does not necessarily mean collecting more and more data elements. Rather, we need to focus on measuring the right things and measuring them well. We must focus on information that increases our understanding of who we are serving and whether the services yield positive outcomes for our clients.
Rachel Solomon is the Executive Director, Performance Improvement at the Centre for Addiction and Mental Health.
